 Health
Health
 Corona Virus
Corona Virus
 Case Fatality Rate
Case Fatality Rate
Don's Home
 Health
Health
 Corona Virus
Corona Virus
 Case Fatality Rate
Case Fatality Rate
| Contact |
Case Fatality Rate (CFR)are the number of deaths divided by the number of confirmed cases. i.e. The probability you will die if you contract COVID-19.
There are 3 main questions regarding the CFR:
2. Why is there so much variance from country to country and location to location.
1. Why is the CFR going down over time.
3. Why is the COVID-19 rate lower than other viruses e.g.MERSA and Ebola
United States:
US 7 day averages
Death peaks lag cases by about 2 weeks:
| Daily | April 10-23 | July 2 - 15 |
|---|---|---|
| Cases | 32,464 | 47,435 |
| Deaths | 2,236 | 760 |
| CFR | 6.9% | 1.6% |

(Click on the chart below for an update)
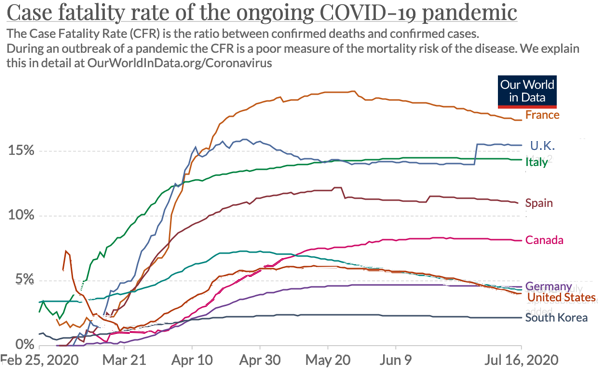
Source: European CDC at Our World in Data
A note on this chart says additional deaths for the US were added at the end of June, hence the higher rate (4%) than I got.
My data came from the US CDC at Worldometer
Why Is the COVID-19 Death Rate Down? - The Atlantic offeres some explanations:
Other:
It is difficult to measure accurately for several reasons.
The number of confirmed cases were low because of testing problems, asymptomatic people and others.
Age and underlying health conditions hypertension (high blood pressure), obesity, chronic lung disease, diabetes mellitus, and cardiovascular disease all increase your risk.
| Japan | 28.2% |
| Italy | 22.8 |
| Germany | 21.4 |
| France | 20.3 |
| Spain | 19.1 |
| United Kingdom | 18.3 |
| Canada | 17.2 |
| United States | 16 |
| Australia | 15.8 |
| New Zealand | 15.3 |
| South Korea | 15.1 |
| Russian Federation | 14.6 |
| Cuba | 14.4 |
We estimated that 45.4% of US adults are at increased risk for complications from coronavirus disease because of cardiovascular disease, diabetes, respiratory disease, hypertension, or cancer.
Rates increased by age, from 19.8% for persons 18-29 years of age to 80.7% for persons >80 years of age, and varied by state, race/ethnicity, health insurance status, and employment.
Data for China indicate that 81% of coronavirus disease (COVID-19) patients had mild cases, 14% had severe cases, and 5% had critical cases (1,2). The overall case-fatality rate (CFR) in China was 3.8% (3), but CFRs were higher for adults with chronic conditions of cardiovascular disease (CVD; CFR 13.2%), diabetes (9.2%), chronic respiratory disease (8.0%), hypertension (8.4%), and cancer (7.6%), compared with 1.4% for patients with none of these conditions (
Another study in China:
According to one study of 45,000 confirmed cases in China, fewer than 1.0% of healthy people who contracted the COVID-19 virus died from the disease.
6.0% for people with cancer, hypertension or chronic respiratory disease, 7.3% for those with diabetes and 10.5% for those with cardiovascular disease. Patients who were 80 or older were also at increased risk, with 14.8% dying.
Deaths per case, which epidemiologists call the "naive" case fatality rate, is a poor measure of the mortality risk, because of undercounting of cases.
At What do we know about the risk of dying from COVID-19? - Our World in Data
They explain the difference between the "case fatality rate", the "crude mortality rate", and the "infection fatality rate", and why they're all different.
They do not explain why the CFR increases over time. See the article below for more on that.
The main problem is the number of "Confirmed" cases, which is reported is much lower than total cases, because of a lack of testing, pre-symptomatic, and non-symptomatic people.
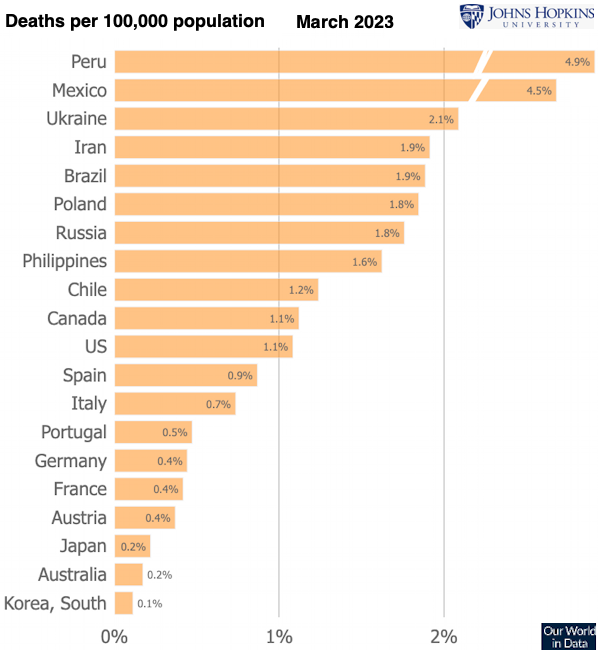
The Crude mortality rate is the number of deaths divided by the population.
The "infection fatality rate", which is what your really want to know. The number of deaths divided by the number infected.
The problem is we don't know the number of infected people, because of the reasons above.
The probability of death is highly dependent on a persons vulnerability, age and underlying health issues, Obesity, Hypertension (High blood pressure), diabetes, respiratory disease, ...
Monitoring trends and differences in COVID-19 casefatality rates using decomposition methods:
Contributions of age structure and age-specific fatality - Max Planck Institute for Demographic Research, Rostock, Germany; Sapienza University of Rome, Italy; Population Research Unit, University of Helsinki, Finland
"CFRs varied from 2.2% in South Korea to
13.0% in Italy. The age-structure of detected cases often explains more than two thirds of crosscountry variation in the CFR. "
" In Italy, the CFR increased from 4.2% to 13.0% between March 9
and April 22, 2020, and more than 90% of the change was due to increasing age-specific casefatality rates. "
"The age structure of confirmed cases has shifted to higher ages, "
" The low contribution of the case age distribution component to the CFR
disparity between South Korea and Germany suggests that these countries might have been more
successful at catching the mild and asymptomatic cases among the younger population groups.
Since then, the CFR of Germany has increased and the age structure of confirmed cases has
shifted to higher ages, and the age structure has become more important in explaining the gap
between South Korea and Germany, making test numbers alone an unlikely explanation for the
different age structure of detected cases. "
" In many countries, only deaths occurring in hospitals are being reported in a timely manner , underestimating the full death count which would include deaths at home and in institutions. Deaths may be underestimated because of a lack of testing both before and after death. Countries might also differ in how they code deaths from underlying or contributory causes ."
Generally, CFRs are highest at the beginning of an infectious outbreak, when the most serious cases are the most readily detected, and declines as testing capacity increases and less serious cases are identified . This has notably not been the case for the COVID-19 epidemic, where the CFR has generally been increasing. Likely this reflects the success of widespread containment measures enacted in response to increasing caseloads. Newly identified cases are increasing more slowly than deaths, despite increases in testing capacity.
"Overall, our results show that differences between countries with low and high CFRs can be driven to a significant extent by the age structure of confirmed cases. Decomposing differences in case-fatality rates over time or between countries reveals important insights for monitoring the spread of COVID-19. An accurate assessment of these differences in CFR across countries and over time are crucial to inform and determine appropriate containment and mitigation interventions, such as social confinement and mobility restrictions. "
Estimated CFR for other diseases SARS-CoV 10% MERS-CoV 34% Seasonal Flu (US) 0.1-0.2% Ebola 2013-16 40%Links: